
Regaining Shoulder Strength Doesn’t Have to Feel Uncertain
If you’re a physical therapist, athletic trainer, or medical provider, you know how often shoulder injuries linger longer than expected. Patients lose motivation. Progress becomes subjective. Without measurable benchmarks, even good therapy can feel like guesswork.
This guide walks through how to rehabilitate a shoulder effectively, following evidence-based frameworks while integrating modern, objective methods that build confidence in both patient and clinician. Whether you’re addressing post-injury recovery or refining performance protocols, you’ll find practical strategies, key phases, and ways to modernize your clinic’s approach.
What We’ll Cover:
- Understanding the Shoulder’s Role in Rehab Success
- Phases of Shoulder Rehabilitation
- Objective Rehab: Bringing Data Into Recovery
- Common Mistakes and How to Avoid Them
- How Technology Is Transforming Shoulder Care
- FAQs About Shoulder Rehabilitation
- When to Integrate Measurable Solutions
Understanding the Shoulder’s Role in Rehab Success
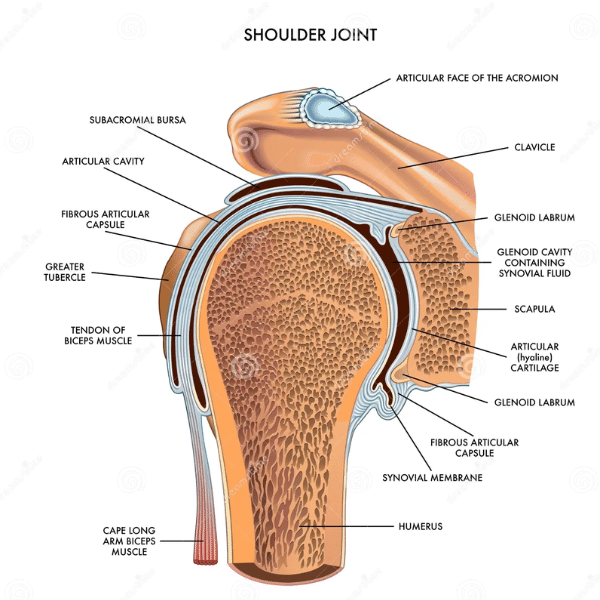
The shoulder is the most mobile joint in the human body, which makes it both powerful and vulnerable. Successful rehabilitation depends on restoring stability and control without compromising movement.
Here’s what that really means:
- Mobility must be earned, not forced.
- Strength should be measured across planes, not just in one direction.
- Functional progress matters as much as pain reduction.
For clinicians, this means evaluating beyond symptoms. True recovery is about measurable improvement in control, strength balance, and load tolerance.
Learn more about the applications of objective rehab for orthopedic physicians.
Phases of Shoulder Rehabilitation
Every recovery follows a pattern, even if the timeline varies. Recognizing and respecting each phase helps keep progress on track and prevents setbacks.

1. Acute Phase: Reduce Pain and Inflammation
Focus on comfort, protection, and gentle movement.
- Use modalities and guided range of motion exercises.
- Maintain mobility in surrounding joints such as the elbow, wrist, and neck.
- Prioritize scapular control and posture.
2. Subacute Phase: Restore Controlled Motion
Once pain subsides, stability and activation become the goal.
- Begin isometric and low-resistance exercises.
- Emphasize rotator cuff and scapular coordination.
- Monitor for compensations that could slow progress.
3. Strengthening Phase: Build Functional Capacity
Now the goal is to regain dynamic control and load tolerance.
- Introduce multiplanar resistance.
- Track strength gains in all directions.
- Start progressive overload carefully.
4. Return-to-Performance Phase: Test, Measure, Refine
Rehabilitation ends when data shows readiness, not when symptoms fade.
- Conduct objective testing and symmetry analysis.
- Simulate sport or job-specific movement patterns.
- Compare results to baselines and clinical standards.
Objective Rehab: Bringing Data Into Recovery
Traditional manual muscle testing can only go so far. It is subjective and often varies between therapists. Data-driven rehab replaces estimation with precision.

Here’s why objective rehab matters:
- Accuracy: Quantifies muscle strength, endurance, and range of motion.
- Motivation: Patients see their progress in numbers, not guesses.
- Consistency: Therapists get repeatable, reliable data across sessions.
- Accountability: Measurable outcomes support referrals and compliance.
Modern clinics now integrate technology to track real-time performance and resistance. Devices like the Humero Tech C1 provide continuous, omnidirectional resistance and live metrics, helping clinicians capture measurable data during sessions.
Common Mistakes and How to Avoid Them
Even well-structured programs can fail if the fundamentals are missed.
1. Rushing Progression
Too much load too soon can lead to compensation and re-injury. Always validate readiness through strength and motion data.
2. Ignoring Scapular Function
A strong rotator cuff means little if scapular mechanics are off. Train both together.
3. Skipping Objective Testing
Without measurable benchmarks, “good enough” becomes the norm. Objective tools help therapists prove improvement and adjust protocols accurately.
4. Overlooking Patient Engagement
Patients lose focus without visible progress. Showing them measurable results helps build trust and motivation throughout recovery.
Explore how data transparency enhances patient benefits.
How Technology Is Transforming Shoulder Care

The future of rehabilitation is measurable, repeatable, and transparent. Clinics adopting technology-backed methods are finding new ways to:
- Quantify improvement session by session.
- Personalize exercise loads dynamically.
- Align with Clinical Practice Guidelines (CPG) for evidence-based care.
- Strengthen referral relationships by demonstrating outcomes.
At Titin KM Biomedical, the Humero Tech C1’s real-time data tracking was designed specifically for this shift. It empowers clinicians with objective data while keeping therapy practical and patient-centered.
Building Trust Through Measurable Expertise
Let’s be honest, rehab can feel uncertain. Patients often wonder if they are actually getting stronger or just “feeling better.” Data takes the guesswork out.
Clinicians who can track and show measurable outcomes stand apart as trusted experts. They attract motivated patients, align with CPG standards, and gain credibility with medical partners.
That is the kind of professional leadership that moves the entire PT field forward. Read what clinics are saying in our testimonials.
Ready to Modernize Your Shoulder Rehab Approach?
If your clinic is ready to bring measurable outcomes into every shoulder rehabilitation session, Titin KM Biomedical can help.
✅ Explore how the Humero Tech C1 features provide real-time resistance and performance tracking to help elevate your rehab outcomes.
✅ Request a Demo to see how innovation meets evidence-based care.
Frequently Asked Questions About Shoulder Rehabilitation
1. How long does shoulder rehabilitation take?
The timeline for shoulder rehabilitation depends on the injury type, severity, and patient consistency. Minor strains or overuse injuries can improve in 6–8 weeks with consistent therapy, while rotator cuff tears or post-surgical recoveries can extend to 4–6 months. What matters most is not the clock but the data. Clinicians should track progressive strength symmetry, range of motion, and endurance levels rather than relying on subjective milestones. When performance metrics and patient function align with pre-injury levels, that is when rehabilitation is complete, not simply when the pain is gone.
2. What are the most effective exercises for shoulder rehab?
There is no one-size-fits-all answer. Effective rehab combines mobility, activation, and strength progressions that reflect the patient’s recovery phase. It’s important to work with a trained professional for your injury recovery.
3. How can I tell if my patient’s rehab is effective?
Effectiveness should be measured, not guessed. Traditional rehab often relies on subjective feedback like “it feels stronger.” Instead, use quantifiable data:
- Measure bilateral strength balance using objective devices.
- Compare objective metric scores session by session.
- Track performance metrics under controlled resistance.
Clinics using measurable outcomes work to not only deliver more consistent recovery but also help reinforce patient trust through visible progress charts and reports.
4. Is technology necessary for good rehab outcomes?
While skilled clinicians remain the cornerstone of recovery, technology now acts as the multiplier of precision and engagement. Devices like the Humero Tech C1 do not replace clinical judgment; they enhance it. By providing continuous resistance and live feedback, therapists get help seeing what is working and where compensation occurs. For patients, real-time visual progress increases motivation and accountability.
5. When should patients return to sport or work?
Returning too soon is one of the leading causes of re-injury. A safe return depends on:
- Pain-free functional movement across all planes.
- Strength symmetry between the injured and non-injured sides
- Endurance and load capacity appropriate to the patient’s sport, job, or activity demands.
Objective performance testing can assist clinicians in assessing readiness and reducing guesswork. When clinicians can quantify output under controlled load using the Humero Tech C1, they can confidently clear patients for full return, knowing strength, endurance, and control have been restored.
6. What if shoulder rehab progress plateaus?
Plateaus happen for a variety of reasons and the key is identifying why. It could be an incomplete activation pattern, an unaddressed scapular imbalance, or simply a lack of measurable progression. This is where data-driven rehab shines. Tracking metrics over time helps pinpoint where the slowdown occurs and helps clinicians to adjust programming precisely. Sometimes, small changes in resistance direction or movement pattern can reignite progress.
Modern Shoulder Rehab: From Guesswork to Measurable Progress
Rehabilitation does not have to be uncertain. By combining structured rehab phases with measurable data, clinicians can support efficient recovery, build trust, and align with evidence-based practice.
If you are ready to modernize your approach, Titin KM Biomedical is here to help clinics like yours turn every shoulder recovery into proof of progress.
Related Reads:
- Objective Muscle Testing vs Manual Muscle Testing
- How Data Builds Patient Confidence in Rehab
- Top Rehab Technologies Elevating Physical Therapy Clinics
- How Long Does It Take to Rehab Shoulder Impingement? - January 19, 2026
- How To Rehabilitate a Shoulder: Modern Strategies for Measurable Recovery - December 11, 2025
- Volleyball and Shoulder Health: The Humero Tech C1 Advantage - November 11, 2025






