If you work with active patients or athletes, you know how quickly a shoulder problem can derail a season, a career, or just everyday life. One awkward dive, extra bullpen session, or weekend tournament, and suddenly they cannot lift, throw, or sleep without pain.
Shoulder rehabilitation in sports medicine is where professionals reconnect the dots between diagnosis, performance demands, and safe return to play. It is more than “a few band exercises.” It is a structured, data informed process that respects tissue healing and the realities of sport.
In this guide, we will break down what shoulder rehab actually means in a sports medicine context, what your patients can expect, and why a professional, technology backed approach delivers better outcomes than DIY routines they find online.
What We’ll Cover:
- How Shoulder Rehabilitation Fits Into Sports Medicine
- Common Shoulder Injuries Treated In Sports Medicine
- What To Expect From Professional Shoulder Rehabilitation
- Why Professional Sports Medicine Rehab Beats A DIY Approach
- When To Seek Shoulder Rehabilitation From A Specialist
- Take The Next Step Toward Healthy, Pain Free Shoulder Movement
How Shoulder Rehabilitation Fits Into Sports Medicine

Shoulder rehabilitation in sports medicine sits at the intersection of injury care, performance, and long term joint health. It is not just about getting pain down. It is about restoring the specific capacity the athlete or active patient needs to compete and live confidently.
At Titin KM Biomedical, we design technology that supports this entire continuum, from early protection after injury to functional, multiplanar loading as athletes near return to sport.
The Goals Of Shoulder Rehabilitation For Active People
For active individuals, the goals of shoulder rehab are broader than simply regaining range of motion. In a sports medicine model, we typically aim to:
- Reduce pain and inflammation to allow quality movement
- Restore full, functional range of motion in all planes
- Rebuild strength and power through the rotator cuff and scapular stabilizers
- Re establish neuromuscular control for overhead, contact, or rotational demands
- Address workload, mechanics, and sport specific risk factors
- Support a safe, confident return to sport with objective benchmarks
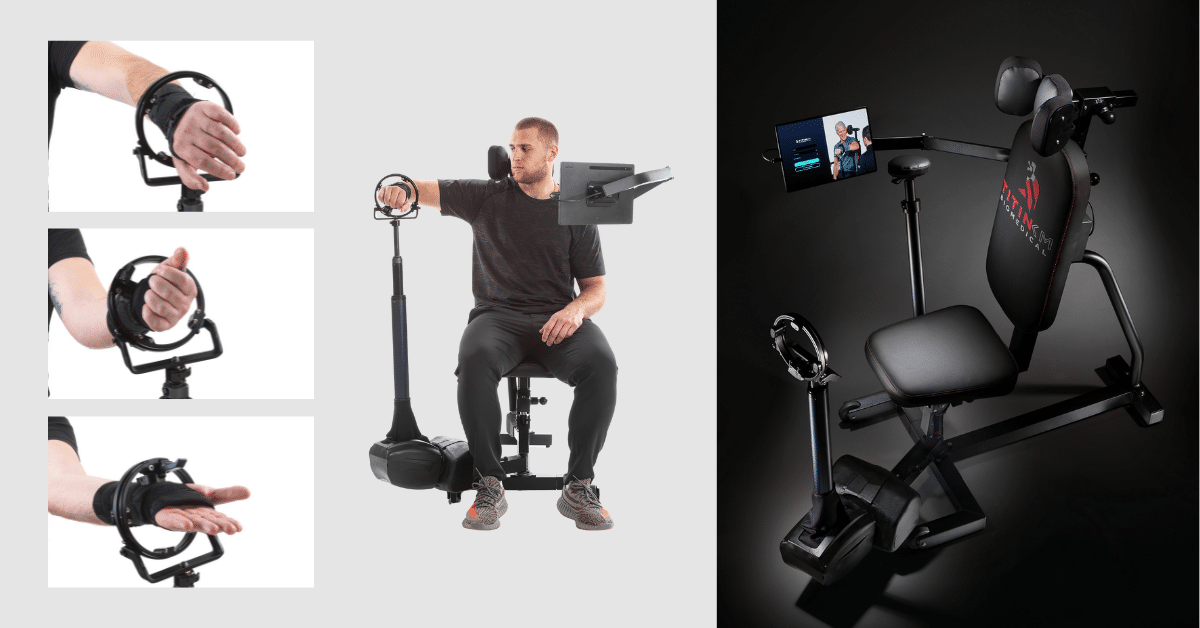
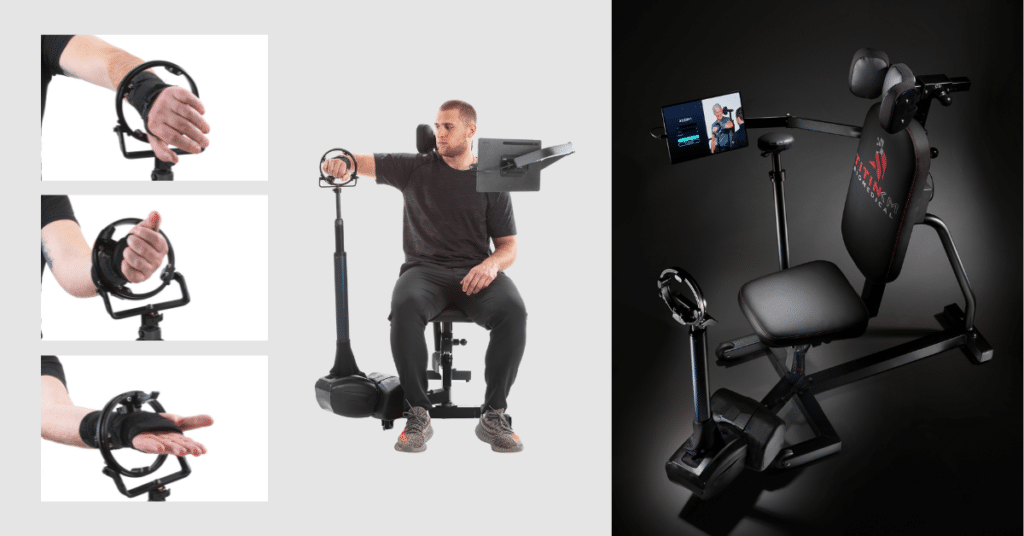
Modern rehab also focuses on patient engagement and clarity. When patients can see measurable progress, they stay invested. That is why we built the Humero Tech C1 as a data driven shoulder rehabilitation device, described in detail in Meet The Humero Tech C1: The Next Gen Tool For Shoulder Rehab.
How Sports Medicine Specialists Approach Shoulder Function
Sports medicine professionals look at shoulder function through a performance lens. They do not just ask “does it hurt” but also:
- Can this shoulder decelerate a throw at game speed?
- Can it tolerate repeated contact or blocking?
- Can it handle the volume and intensity of a full season?
That is why objective data matters. With technology like the Humero Tech C1, which uses continuous omnidirectional resistance and live metrics, they can assess:
- Strength and endurance in multiple planes
- Symmetry between sides
- Control through mid and end range
If you want a deeper dive on how this style of resistance and analysis supports shoulder tissue and neuromuscular control, here are more details in The Science Behind Omnidirectional Resistance In Shoulder Therapy.
Common Shoulder Injuries Treated In Sports Medicine
In sports medicine, there are patterns. Certain sports and positions tend to drive specific shoulder injuries. Good rehabilitation starts with understanding the underlying mechanism, tissue involved, and performance demands that will stress that tissue again.
Overuse Injuries Of The Rotator Cuff
Throwing athletes, swimmers, volleyball players, and weightlifters frequently develop rotator cuff irritation from repetitive overhead loading. Clinically, that can show up as:
- Deep ache after activity
- Pain with reaching or lifting
- Weakness or early fatigue
Rotator cuff rehab focuses on restoring tendon capacity, improving scapular mechanics, and managing workload. Using data informed resistance, can progressively challenge these tissues in safe planes instead of guessing. For an example in volleyball athletes, see Volleyball And Shoulder Health: The Humero Tech C1 Advantage.
Instability, Dislocations, And Labral Tears
Contact sports, collision with the ground, or a single high force event can cause shoulder instability or labral damage. These patients often report:
- Feeling of the shoulder “slipping” or “giving way”
- Apprehension with certain positions, especially abduction with external rotation
- History of dislocations or subluxations
Rehabilitation here is precision work. They must progressively load the dynamic stabilizers while protecting vulnerable positions early on. For some patients, this is post surgical: for others, conservative management with strict progressions is appropriate.
Tendonitis, Bursitis, And Impingement Syndromes
Many active adults arrive with broad labels like tendonitis, bursitis, or impingement. In practice, they present with:
- Painful arc when lifting the arm
- Night pain on the affected side
- Stiffness after inactivity
These cases benefit from a structured progression that addresses strength deficits, motor control, and activity modification. Using technology that allows adjustable resistance and multiplanar patterns, in Elevating Shoulder Health: How Adjustable Resistance With Humero Tech C1 Helps Enhance Rehab & Prevention, professionals can learn how to fine tune loading without flaring symptoms.
Post Surgical Shoulder Rehabilitation
After rotator cuff repair, labral repair, or capsular tightening procedures, sports medicine rehab must respect healing timelines while preventing stiffness and deconditioning.
Typical priorities include:
- Protecting the repair in early phases
- Guiding safe passive and active assisted motion
- Reintroducing strength in gradual, measured stages
- Planning realistic, sport specific return to play milestones
In any surgical case, objective data and clear communication between surgeon, therapist, and athletic staff are critical.
What To Expect From Professional Shoulder Rehabilitation
When a patient enters a sports medicine environment for shoulder rehab, the process should feel organized, intentional, and tailored. It is not a generic “three sets of ten” program printed from a template.

Comprehensive Evaluation And Movement Analysis
Medical professionals start by listening. History gives us insight into training load, sport demands, and prior injuries. Then they perform a detailed assessment that may include:
- Range of motion testing
- Strength and endurance measurements
- Functional tests like closed chain stability, overhead control, or throwing mechanics
- Palpation and special tests guided by best practice
With tools like the Humero Tech C1, clinicians gain access to objective strength and control metrics. These can help support clinical reasoning and patient education, as detailed in our overview of Clinical Benefits.
Personalized Treatment Planning For Your Sport And Lifestyle
A swimmer does not need the same rehab plan as a catcher or a weekend skier. Once the clinical picture is understood, professionals build a plan around:
- Tissue healing stage
- Sporting position or role specific demands
- Volume and intensity of training or work
- Equipment and environment available
Sports medicine clinics that adopt advanced shoulder equipment, like those described in Why Forward Thinking Clinics Choose Advanced Shoulder Rehab Equipment, can match exercise selection and loading to those real world demands instead of approximating them.
Hands On Techniques And Targeted Therapeutic Exercise
Professional rehab blends skilled manual therapy with targeted exercise and patient education.
Depending on the diagnosis and phase, care may include:
- Joint and soft tissue techniques to reduce pain and improve mobility
- Neuromuscular training for scapular and rotator cuff coordination
- Strength and power work using bands, free weights, cables, or smart resistance
- Closed chain drills for stability and proprioception
In working with PT clinics and sports programs, the best results are when exercises are not only well chosen, but also informed by data. Data driven resistance systems allow therapists to progress or pull back with confidence instead of guessing.
Progress Monitoring And Return To Sport Planning
Progress should be visible, not vague. In a sports medicine setting, regularly reassess:
- Pain levels and functional limitations
- Objective strength and endurance
- Range of motion and quality of movement
- Sport specific skills such as throwing speed or volume tolerance
Return to sport is then based on criteria, not the calendar alone. We outline how this technology supported approach protects athletes in Preventing Re Injury: The Role Of Data Driven Rehab In Shoulder Health.
Why Professional Sports Medicine Rehab Beats A DIY Approach
Many patients now arrive having tried “internet rehab” plans or random exercise videos. While motivation is good, unstructured self directed rehab can often create bigger problems than it solves.

Risks Of Self Directed Shoulder Rehab
On paper, DIY rehab looks simple. In reality, the shoulder is complex, and guesswork can be risky. Common pitfalls include:
- Doing too much, too soon, and aggravating tissue
- Choosing exercises that do not match the diagnosis or deficits
- Loading in unsafe positions after instability or surgery
- Masking symptoms instead of addressing underlying causes
In overhead and contact athletes, poor self management can set the stage for chronic problems and lost seasons. Explore how traditional, non objective methods can hold patients back in Why Traditional Shoulder Rehab Methods May Be Holding Your Patients Back.
Advantages Of Working With A Sports Medicine Team
A sports medicine team brings structure, experience, and technology to the table. When patients work with us or with clinics using tools like the Humero Tech C1, they benefit from:
- More accurate diagnosis and clear explanation of findings
- Phased loading plans that respect tissue healing
- Real time feedback and data on strength and control
- Collaboration between physicians, therapists, and athletic trainers
This kind of support is especially important for higher level athletes. Our partners in Sports Medicine Applications use objective rehab data to help inform smarter decisions about practice progression, pitch counts, and contact exposure.
Building Long Term Shoulder Strength And Injury Prevention
Good shoulder rehabilitation does not end when pain fades. Athletes need to build long term resilience, particularly in high demand sports like baseball, football, and volleyball.
Using adjustable resistance and multiplanar training, can:
- Address side to side asymmetries
- Build endurance for long seasons
- Strengthen decelerators and stabilizers that often get neglected
This prevention mindset is why many organizations now integrate tools like the Humero Tech C1 into both rehab and performance programs, as outlined in Maximizing Athletic Careers: Humero Tech C1 For Recovery, Prevention & Peak Performance.
When To Seek Shoulder Rehabilitation From A Specialist
Knowing when to involve a sports medicine rehab team can be the difference between a short, clean recovery and a nagging, season long issue.
Warning Signs You Should Not Ignore
Medical providers, coaches, and athletes are encouraged to take shoulder symptoms seriously, especially when you notice:
- Pain that lasts more than a few days or worsens with activity
- Night pain that disrupts sleep
- Loss of strength or visible asymmetry
- Sense of instability, “slipping,” or catching
- Inability to perform key sport tasks at normal intensity
These are red flags that warrant a structured evaluation rather than waiting or self treating.
How Quickly To Act After An Injury Or Flare Up
For acute injuries like dislocations, traumatic falls, or clear loss of function, rapid assessment is non-negotiable. For overuse patterns, early intervention is still recommended once symptoms are consistent or performance drops.
Early referral allows providers to:
- Confirm or refine diagnosis
- Set load management guidelines
- Start gentle, appropriate motion and activation
- Plan imaging or specialist consults when indicated
Our work with Orthopedic Physicians and hospitals shows that coordinated care and early objective testing shorten the time to accurate treatment.
What To Bring And How To Prepare For Your First Visit
When a patient arrives for a sports medicine shoulder evaluation, they will get more value if they come prepared. Typically suggest they bring:
- Imaging reports and prior medical records
- A list of medications and relevant health history
- Information about sport, position, and current training volume
- Any braces or equipment they use for the shoulder
Professionals also like to know their specific goals, whether that is returning to a pro level or lifting a grandchild comfortably. That context helps us build a rehabilitation plan that fits their real life demands, view more of our Patient Benefits resources.
Medical Disclaimer: The information provided in this article is for educational and informational purposes only and is not intended as medical advice. It should not be used to diagnose, treat, cure, or prevent any medical condition. Always consult with a qualified healthcare professional regarding any medical concerns, symptoms, or treatment decisions.
Take The Next Step Toward Healthy, Pain Free Shoulder Movement
Shoulder rehabilitation in sports medicine is not a one size fits all protocol. It is a structured, evidence guided process that blends expert clinical reasoning with modern equipment and clear, measurable goals.
When clinics and sports organizations work with technology like the Humero Tech C1, they gain a tool that:
- Provides continuous omnidirectional resistance for multiplanar training
- Delivers real time performance data to help inform decisions
- Engages patients by making progress visible session to session
We are proud to support PT clinics, sports medicine programs, hospitals, and academic centers that want to raise their standard of shoulder care. Our mission and story are outlined in Our Mission, and you can see how peers are using this technology in our growing library of Patient Outcomes.
What A Typical Rehab Journey Looks Like
While every case is unique, a technology supported sports medicine shoulder journey often follows this arc:
- Evaluation and baseline testing Clinical assessment paired with objective strength and control data.
- Early phase protection and motion Respect healing while maintaining safe range and activation.
- Progressive loading Gradually build strength and endurance with quantifiable changes in resistance and volume.
- Sport specific integration Rehearse the patterns and speeds the athlete needs in their sport.
- Criteria based return to play Decisions grounded in objective benchmarks, not guesswork.
We go deeper into the broader evolution of these methods in The New Gold Standard In Shoulder Rehab.
How To Get Started With A Sports Medicine Shoulder Evaluation
If you are a medical provider or part of a sports organization, the first step is making sure your athletes have access to objective, modern shoulder rehabilitation instead of relying on outdated manual testing or generic exercise sheets.
We partner with PT clinics, sports medicine practices, college and pro teams, and health systems to bring the Humero Tech C1 into their environment. To explore how this technology can fit your setting, visit our main site at Titin KM Biomedical or connect with our team through the information on our Contact Us page.
Related reads:
For a deeper look at how advanced equipment shapes modern shoulder care, you might also be interested in our articles on:
- What Equipment Is Needed For Modern Shoulder Rehab
- The Role Of Equipment In Speedy Shoulder Rehab
- From Prevention To Recovery: The Objective Shoulder Rehab Device You Need
Each piece builds on the same idea that has driven our work from the beginning: better data, improved engagement, and supported outcomes for every shoulder recovery.
Key Takeaways
- Shoulder rehabilitation in sports medicine is a structured, data-informed process that connects accurate diagnosis, sport demands, and a safe, criteria-based return to play.
- Modern shoulder rehab goes beyond pain relief to restore full range of motion, strength, neuromuscular control, and sport-specific capacity for active patients and athletes.
- Sports medicine specialists use tools like the Humero Tech C1 to provide omnidirectional resistance and objective metrics, allowing precise loading and progress tracking throughout rehab.
- Professional shoulder rehabilitation sports medicine programs significantly outperform DIY routines by matching exercises to the exact injury, healing stage, and sport demands while reducing the risk of re-injury.
- Early referral to a sports medicine shoulder specialist after injury, persistent pain, instability, or loss of function can help shorten recovery time and support long-term shoulder health and performance.
Frequently Asked Questions About Shoulder Rehabilitation in Sports Medicine
Frequently Asked Questions About Shoulder Rehabilitation in Sports Medicine
- What Is Shoulder Rehabilitation In Sports Medicine? - February 2, 2026
- How Long Does It Take to Rehab Shoulder Impingement? - January 19, 2026
- How To Rehabilitate a Shoulder: Modern Strategies for Measurable Recovery - December 11, 2025